The TVM procedure
What follows is a total new concept in Gynaecology prolapse surgery, ok, not totally new: it’s rather a progression of previous practised operations. It’s in my mind bringing together different techniques used already.The operation that I’m about to describe can only be done by an experienced Pelvic floor surgeon: it falls in the super specialisation field of Urogynaecology, and not in the hands of a general gynaecologist. At this moment only a handful of Pelvic floor gynaecologists can do this procedure, but I’m convinced that it will be done within a year by most, if not all. It is developed in France and the main training schools are located there.
Prolapse of the pelvic floor is more common in women than one realise: figures as high as 30% is been reported in women after the menopause. It can also be present in the younger women.
A genetic preposition gives rise to the weakening of the supportive tissue of the pelvic organs leading to sagging of the pelvic organs into the vagina. Childbirth may have a role to play (giving rise to the idea in some centres that a caesarean section may protect you against this happening in later life - an idea not supported by everyone) as the loss of the “protection” of the female hormone (estrogens), giving the postmenopausal era the highest incidence. Listening to these unfortunate women one will hear about precipitous labours (over and done within hours!), and also that mother, aunts, and grandmothers had the same problem (genetic).
What in effect happens is that the support of the bladder, rectum and uterus, given by the vaginal fascia, are not present, and everything falls into the vaginal hiatus. This happens in most cases over time and the onset of symptoms is usually insidious. In severe cases the whole vagina can turns inside out and hang outside the body.
What can be done? The pelvic wall consists of basically muscles and layers of fascia (that’s apart from the bony frame - the sacrum at the back and the iliac bones on the sides). The integrity of these soft tissues keep the pelvic organs (internal genitalia, bladder and rectum) inside the pelvis, or shall one say, outside the vagina? With weakening of these supports one can increase the muscular tone via physiotherapy, but these help only partially. The use of pessaries has only a limited role to play.
A surgical approach is thus indicated. The weakened tissues (fascia) is usually overstretched and can be tightened, or extra tissue (synthetic or biological) can be build in.
What in effect happens is that the support of the bladder, rectum and uterus, given by the vaginal fascia, are not present, and everything falls into the vaginal hiatus. This happens in most cases over time and the onset of symptoms is usually insidious. In severe cases the whole vagina can turns inside out and hang outside the body.
What can be done? The pelvic wall consists of basically muscles and layers of fascia (that’s apart from the bony frame - the sacrum at the back and the iliac bones on the sides). The integrity of these soft tissues keep the pelvic organs (internal genitalia, bladder and rectum) inside the pelvis, or shall one say, outside the vagina? With weakening of these supports one can increase the muscular tone via physiotherapy, but these help only partially. The use of pessaries has only a limited role to play.
A surgical approach is thus indicated. The weakened tissues (fascia) is usually overstretched and can be tightened, or extra tissue (synthetic or biological) can be build in.
By only using a tightening technique one use the same tissue that was stretched in the first place, and with time it will stretch again! The answer will thus lie in the use of extra tissues from outside the body.
Up to now an abdominal approach is recognized as the golden standard of surgical treatment: with this the top of the vagina is pulled and hooked onto the sacral promontory by means of a synthetic mesh (called: sacro-colpopection).The morbidity is unfortunately extremely high with this method with a quite few days of hospitalization, sometimes with a short stay in the ICU.
The problems with sacro-colpopections lead to avenues into other methods, especially through a vaginal approach to the repair of the pelvic floor defects, with the use of direct stitching of a defect in the wall (paravaginal vaginal repair) or the introduction of synthetic or biological membranes into the defective fascia layers. Sometimes a combination of these were done.
A new innovative technique was introduced this year from France which could be the answer to our prayers. It is in short a complete product that consists of a synthetic mesh that is introduced via a keyhole incision in the vagina onto the pelvic floor and thereby supporting the pelvic organs at the spot where the fascia is weakened, namely on the vaginal wall’s fascia lining.
This procedure is called a TVM (Tensionfree Vaginal Mesh): manufactured as the Prolift system by Gynecare. When it is put into the anterior vaginal wall it’s called an Anterior TVM, and into the posterior wall, a Posterior TVM.
How does it work? The whole vaginal wall is being dissected loose from the underlying fascia and this mesh is introduced onto the layer, at the back between the vagina and rectum and in front between the bladder base and the vagina.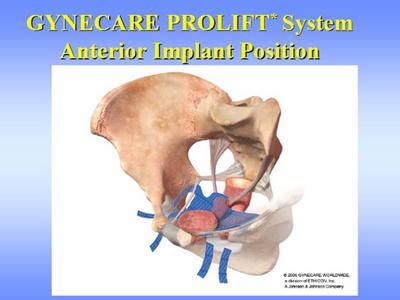
For the Anterior TVM a small 4 cm incision is made 2 cm proximal of the cervix on the anterior wall of the vagina. Through this keyhole the bladder is loosened by sharp dissection from the vaginal wall, first in the midline towards the urethra (bladder base) – the dissection begins thus in the deep and come forward towards the surgeon, and then towards the sidewalls of the pelvis, through the attachments of the fascia on the pubic rami on the sidewalls until the whole of the side holes (Obturator foramina= see pictures) of the pelvis is free on the inside: proper knowledge of the anatomy of the pelvis and experience in vaginal surgery is essential.
With the whole bladder loose from the surrounding pelvic tissues, the mesh can be brought through the keyhole in the vagina and with a special technique four bands (two on each side) are being pulled through the side holes (Obturator foramina) of the pelvic bone:
Imagine a huge H and turns it sideways. The two points goes through these openings, two at each side. The cross bar of the H is broad and lies under the bladder base and support the bladder. The bladder hangs now on this hang mat that pulls it away from the vaginal wall and upwards, supporting the bladder.
A new innovative technique was introduced this year from France which could be the answer to our prayers. It is in short a complete product that consists of a synthetic mesh that is introduced via a keyhole incision in the vagina onto the pelvic floor and thereby supporting the pelvic organs at the spot where the fascia is weakened, namely on the vaginal wall’s fascia lining.
This procedure is called a TVM (Tensionfree Vaginal Mesh): manufactured as the Prolift system by Gynecare. When it is put into the anterior vaginal wall it’s called an Anterior TVM, and into the posterior wall, a Posterior TVM.
How does it work? The whole vaginal wall is being dissected loose from the underlying fascia and this mesh is introduced onto the layer, at the back between the vagina and rectum and in front between the bladder base and the vagina.
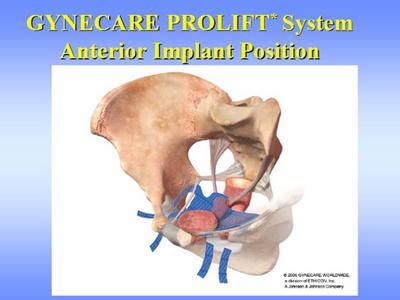
For the Anterior TVM a small 4 cm incision is made 2 cm proximal of the cervix on the anterior wall of the vagina. Through this keyhole the bladder is loosened by sharp dissection from the vaginal wall, first in the midline towards the urethra (bladder base) – the dissection begins thus in the deep and come forward towards the surgeon, and then towards the sidewalls of the pelvis, through the attachments of the fascia on the pubic rami on the sidewalls until the whole of the side holes (Obturator foramina= see pictures) of the pelvis is free on the inside: proper knowledge of the anatomy of the pelvis and experience in vaginal surgery is essential.
With the whole bladder loose from the surrounding pelvic tissues, the mesh can be brought through the keyhole in the vagina and with a special technique four bands (two on each side) are being pulled through the side holes (Obturator foramina) of the pelvic bone:
Imagine a huge H and turns it sideways. The two points goes through these openings, two at each side. The cross bar of the H is broad and lies under the bladder base and support the bladder. The bladder hangs now on this hang mat that pulls it away from the vaginal wall and upwards, supporting the bladder.
Within two days the surrounding tissue reaction of the body will lead to ingrowths of connective tissues into this mesh and in due course will incorporate the mesh into a new fascia layer. A weak spot is corrected!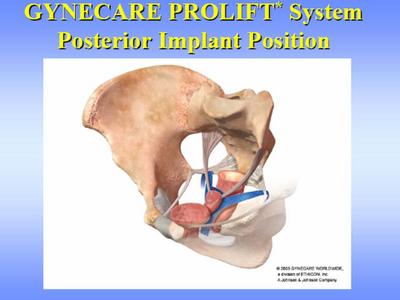
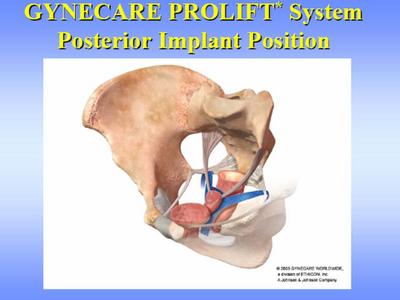
For a Posterior TVM the rectum are being loosened from the posterior vaginal wall through two transverse vaginal incisions, one at the bottom and one just to the back of the cervix. Once again: the whole vaginal wall is being loosened from the surrounding pelvic wall and bones.
A pulley system are used whereby two bands go from the sides of the anus upwards towards the sacrum, hooked around ligaments (the sacro-spinous ligaments) and come down towards the cervix into a broad mesh that lies over the front part of the rectum between the vagina and rectum. This mesh is anchored at the top on the uterus and at the bottom on the fibrous body between the opening of the vagina and the anus (perineal body). By pulling on the bands where it come out laterally of the anus the top part goes up via the pulley and thus straightened the back wall of the vagina and the uterus are being replaced to it’s proper position.
the etceteras of posterior repairs
A pulley system are used whereby two bands go from the sides of the anus upwards towards the sacrum, hooked around ligaments (the sacro-spinous ligaments) and come down towards the cervix into a broad mesh that lies over the front part of the rectum between the vagina and rectum. This mesh is anchored at the top on the uterus and at the bottom on the fibrous body between the opening of the vagina and the anus (perineal body). By pulling on the bands where it come out laterally of the anus the top part goes up via the pulley and thus straightened the back wall of the vagina and the uterus are being replaced to it’s proper position.
This operation is done only through 3 holes of 4 cm each in the inside of the vagina! No hysterectomy is necessary, it can be done with a local anaesthetic (e.g. spinal block), it takes only 80 minutes and NO pain is felt afterwards. The patient can go home as soon as 24 hours after the procedure, with the mean hospital time 3 days.
Her buttocks will be blue (but so is the queen’s!) for a few days, and that’s it!
Her buttocks will be blue (but so is the queen’s!) for a few days, and that’s it!
Kijk na de volgende plaatjes om de chirurgie beter te begrijpen/ Slides of this Prolift system is available on:
http://photobucket.com/albums/a372/bekkenbodem/POP%20Chirurgie/
password: "andri"
(AJN)
http://photobucket.com/albums/a372/bekkenbodem/POP%20Chirurgie/
password: "andri"
(AJN)
Please feel free to ask questions, or give your own opinions or ideas regarding this problem unique to women.




2 Comments:
There are two points that occur to me initially.
1. You make no mention of prolapse due to sloppy surgery during hysterectomy, ie none re-attachment.
2. What would happen if the material was rejected, particularly after the bladder had been separated from the surrounding fascia?
to begin with point 2:
a very valid point. Rejection of the mesh will always be a great fear.I do not think that rejection as seen in tissue rejection will happen if one uses the synthetic materials, maybe with xeno or allographs, but even then it is a distant occurence- the tissue used is without any dna or proteien substances. Infection and it´s associated problems is to my mind a greater fear and danger. The disection of the bladder from it´s surrounding supports are necessary in any type of paravaginal repair: if not done properly the repair can not been done properly. I always fear that this can leads to neuroligacal " denuding" the bladder with secondary sequelae due to this. I stay clear from the bladder pillars, but some colleques even cut the bladder pillars too, with no ill effects.
What I found amazing is how the vaginal skin adhere to the underlying tissue without any specific tying down stiches: We were taught that extra skin must be removed before one re-suture the vaginal cut. In the paravaginal repairs, and especially with the tensionfree vaginal mesh applications, this is not done . At the end of the procedure a whole loose sac remains: by simply plugging the vagina and thus pushing this sac onto the underlying tissue ( and mesh) for 48 hours, the vagina remodeled itself into the normal form. I can look now back to my first year using these meshes and paravaginal disections well onto the inside of the obturator foramina and freeing the whole whiteline from top to bottom, with an end result of a looselying vaginal skin: and assesing these anatomies 6 weeks and even 6 months later. I still am amazed at the fantastic anatomical results of this.
Looking outof this perspective one do wonder if post hysterectomy tying and anchoring or re- attaching of the vagina onto underlying ligaments have any effect.
Having said this: I still like to use the utero sacrals as anchors to the vaginal top during my hysterectomies!
Post a Comment
<< Home